• Global distribution issues continue to be at the forefront, particularly as more pharmaceutical and biopharmaceutical firms ship temperature-sensitive products worldwide. Speakers called for greater cooperation among firms at all points along the distribution chain, from suppliers to manufacturers to third-party logistics firms, and to end-users such as pharmacies and hospitals. The “last-mile”portion of the distribution chain, where packaged product reach the end user and individual patient, is an area of concern in terms of keeping the product at the correct temperature.
• Validation and qualification were used and possibly misused by many speakers and attendees. As the conference moved forward, the general viewpoint was that validation is an appropriate term for a process conducted in a controlled environment, typically at the point of manufacture. Once packaged product is shipped from the manufacturing site, a process would be considered qualified. That view was espoused by Rafik H. Bishara, chair for the Pharmaceutical Cold Chain Discussion Group, an active working group of the Parenteral Drug Assn.. Depending on the specific process, the recommendation here is to first seek assistance from the Food and Drug Administration.
• Considerable attention was given to the subject of excursions, or temperature fluctuations during transport and storage that can affect drug product stability. The most challenging shipping temperature range continues to be in the 2º to 8º C range, which is the common range for product kept in a refrigerator. A good definition of the effects of temperature excursions on mean kinetic temperature and shelf life can be found online at this link. This site is a service of the National Library of Medicine and the National Institutes of Health.
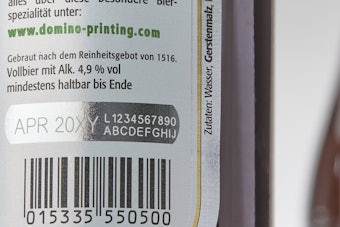
• Cold Chain exhibitors showcased insulated containers, refrigerants, temperature and humidity indicators, data loggers, storage and courier services, nested boxes, and phase-change products to maintain or monitor temperatures of packaged products in transit, be they by air, land, or sea. Often, these monitoring devices track temperature and time, and can be linked to a computer so that the drug or biologic manufacturer can track temperatures. Warning lights or signals indicate if a temperature excursion exists. That allows the manufacturer to take appropriate action to rectify the situation. Doing so can be critical. For example, a pallet load of product can be worth millions of dollars. If it's subjected to unacceptable temperatures, it may no longer be effective, and possibly be dangerous.
• Dr. In K. Mun, Ph.D., and director of biomedical research with HCP, Inc., an operator of hospitals and health systems, referred to the cold chain “as more of a problem than a business opportunity.” He noted that although hospitals have worked hard and invested considerable financial resources to reduce medication errors, “hospitals have difficulty admitting mistakes with lawyers all around.” He said bar coding and RFID are being used more frequently, but there is much progress to be made. Mun said it's the hospital that gets hit first when a patient gets sick or dies from a medication error, but Bishara pointed out that “the hospital will have a major partner,” referring to the medication manufacturer whose name is printed on the bottle or package.
• Consider prechilling product and packaging components, particularly those in the 2º to 8º C temperature range, suggested Kristine Marchant, senior director, materials management with Acambis, the biotech company that recently completed a U.S. government contract to create a national stockpile of vaccines to treat a possible smallpox outbreak in the event of bioterrorism. Similar to Bishara, Marchant said that a validated package can be tested in a laboratory environment, whereas qualification of a package would be done during shipping and transportation, where the company can't control the process.
For more information on the conference, visit this page.